
What is Dementia?
Rather than a specific disease, dementia is a general term describing a decrease in cognitive functions such as thinking, reasoning, or remembering. Changes in mood and behavior are common in individuals experiencing dementia, dementia can also be severe enough to reduce an individual’s ability to perform everyday tasks. There are 10 different forms of dementia. Alzheimer’s disease is the most common and well-known, it accounts for 60 to 80 percent of all dementia cases. Vascular dementia, which occurs after a stroke, is the second most common form. Symptoms of dementia may also result from other conditions, including some that are reversible, such as thyroid problems and vitamin deficiencies.
What are the Symptoms of Dementia?
Because dementia is a result of injury to the brain, the symptoms displayed can vary based on the location and extent of the injury as well as the condition causing the injury. Symptoms of dementia are often mild initially but worsen over time. Common signs and symptoms of dementia may include:
- difficulty recalling recent events
- difficulty making decisions, solving problems, carrying out a sequence of tasks (such as cooking a meal), or concentrating
- difficulty following a conversation or finding the right word
- problems judging distances or seeing objects in three dimensions
- losing track of the day or date, or becoming confused about where they are
- sudden mood changes or strong emotions, including feeling frustrated, irritable, withdrawn, anxious, easily upset, or unusually sad seeing things that aren’t there (visual hallucinations) or believing things that aren’t true (delusions)
While it is a common symptom of dementia, memory loss alone does not indicate that a person has dementia. Doctors diagnose dementia only if two or more brain functions such as memory, language skills, perception, or cognitive skills are significantly impaired without loss of consciousness. Symptoms tend to develop slowly and progress to a potentially debilitating state. Initial symptoms may appear as mild memory loss but can progress until the individual is unable to interact with others or their environment.

How Common is Dementia?
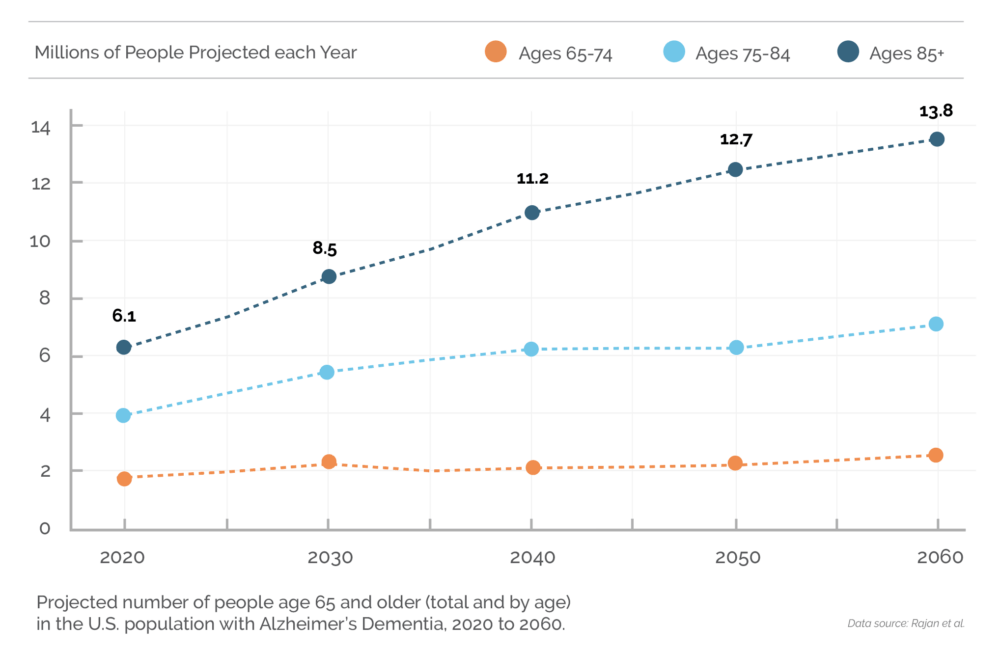
Today, one in three seniors dies from a form of dementia. Deaths from Alzheimer’s have more than doubled between 2000 and 2019, and it is predicted that by 2050, 13 million Americans will be living with Alzheimer’s disease. In fact, an estimated 6.7 million Americans aged 65 and older are living with Alzheimer’s dementia in 2023. Seventy-three percent are age 75 or older and of the total U.S. population about 1 in 9 people (10.8%) age 65 and older has Alzheimer’s dementia. The percentage of people with Alzheimer’s dementia increases with age: 5.0% of people aged 65 to 74, 13.1% of people aged 75 to 84, and 33.3% of people age 85 and older have Alzheimer’s dementia. Even people younger than 65 can also develop Alzheimer’s dementia. Although prevalence studies of younger onset dementia in the United States are limited, researchers believe about 110 of every 100,000 people ages 30-64 years, or about 200,000 Americans in total, have younger-onset dementia.
How Can Dementia Be Prevented and Treated?
While there are multiple forms of dementia, Alzheimer’s is the most common. The number one risk factor for Alzheimer’s is aging, particularly for individuals 65 years or older. However, Alzheimer’s is not a normal stage of aging and while less common, the disease can develop in adults aged 40-50. There is no cure for Alzheimer’s. Modern medical treatments may help slow the progression of the disease, increasing longevity and quality of life. Those with Alzheimer’s live an average of eight years after their symptoms become noticeable to others, but survival can range from four to 20 years depending on age and other health conditions. Current research is focused on the prevention of Alzheimer’s as well as early detection and medication. Researchers are also dedicating significant time and resources to evaluating the role that diet, exercise, and social connections may have in the prevention of dementia. Despite not having a cure there are areas of opportunity to delay or support those with dementia through diets, exercise, and how food is presented to individuals.
Nutritional Approaches
Diet has gained increasing interest as a target for developing preventive opportunities against dementia, as it impacts several mechanisms underlying dementia, including oxidative stress, inflammation, and vascular abnormalities. Accordingly, various studies have linked adherence to healthy dietary patterns to a slower rate of cognitive decline and a decreased risk of dementia. The Memory and Aging Project found that better MIND diet adherence was associated with a lower risk of Alzheimer’s dementia and in The Personality and Total Health Through Life Study, persons who better adhered to the MIND diet were less likely to have all-cause dementia or mild cognitive impairment 12 years after baseline. Therefore, the Mediterranean-Dietary Approaches to Stop Hypertension (DASH) Intervention for Neurodegenerative Delay (MIND) diet has been developed, to uniquely emphasize foods linked to brain health, such as green leafy vegetables and berries. MIND diet is a hybrid of the Mediterranean and Dietary Approaches to Stop Hypertension (DASH) diets, and it has shown promise for preventing cognitive decline and maintaining brain health. A traditional Mediterranean diet primarily consists of grains, legumes, vegetables, fruit, nuts, and fish. The DASH diet emphasizes fruit, vegetables, and low-fat dairy products. Adherence to the MIND diet has indeed been linked to better cognitive performance, less cognitive decline, and lower dementia risk.

Dining Approaches
During the middle stages of Alzheimer’s, distractions, too many choices, and changes in perception, taste, and smell can make eating more difficult. According to the Alzheimer’s Association, the following tips can help:
- Limit distractions. Serve meals in quiet surroundings, away from the television and other distractions.
- Keep the table setting simple. Avoid patterned plates, tablecloths, and placemats that might confuse the person. Using color to contrast plates against a tablecloth or placemat can make it easier for the person to distinguish the food from the plate or table.
- Provide only the utensils needed for the meal to avoid confusion.
- Distinguish food from the plate. Changes in visual and spatial abilities may make it tough for someone with dementia to distinguish food from the plate or the plate from the table. It can help to use white plates or bowls with a contrasting color placemat. Avoid patterned dishes, tablecloths, and placemats.
- Check the food temperature. A person living with dementia might not be able to tell if something is too hot to eat or drink. Always test the temperature of foods and beverages before serving.
- Offer one food item at a time. The person may be unable to decide among the foods on his or her plate. Serve only one or two items at a time. For example, serve mashed potatoes followed by the main entree.
- Be flexible with food preferences. It is possible the person may suddenly develop certain food preferences or reject foods he or she may have liked in the past.
- Allow plenty of time to eat. Keep in mind that it can take an hour or more for the person to finish.
- Eat together. Give the person the opportunity to eat with others. Keeping mealtimes social can encourage the person to eat.
- Keep in mind the person may not remember when or if he or she ate. If the person continues to ask about eating breakfast, consider serving several breakfasts — juice, followed by toast, followed by cereal.
During the middle stage of Alzheimer’s, allow the person with dementia to be as independent as possible during meals. A few suggestions as follows:
- Make the most of the person’s abilities. Adapt serving dishes and utensils to make eating easier. You might serve food in a bowl instead of on a plate or try using a plate with rims or protective edges. A spoon with a large handle may be less difficult to handle than a fork, or even let the person use his or her hands if it’s easier.
- Serve finger food. Try bite-sized foods that are easy to pick up, such as chicken nuggets, fish sticks, tuna sandwiches, orange segments, steamed broccoli, or cauliflower pieces. Or make a meal in the form of a sandwich to make it easier for the person to serve him or herself.
- Try hand-over-hand feeding. Demonstrate eating behavior by putting a utensil in the person’s hand, placing your hand around theirs, and lifting both of your hands to the person’s mouth for a bite.
- Don’t worry about neatness. Let the person feed himself of herself as much as possible. Set bowls and plates on a non-skid surface such as a cloth or towel. Use cups and mugs with lids to prevent spilling. Fill glasses half full and use bendable straws.

The NEXDINE Difference
As the SVP of Nutrition Health and Wellness and Certified Dementia Practitioner, I truly believe that NEXDINE Hospitality dining programs support the dementia population of our business significantly. NEXDINE supports the use of the MIND diet when creating each account’s memory care menus. With NEXDINE’s Culinary Commitments, our culinary teams have full disposal of the ingredients to create recipes and menus that adhere to the MIND standards. The NEXDINE program encompasses all aspects of residents’ and patients’ needs throughout the disease progression from adequate hydration, increased nutritional needs, altered textures, and finger food. In addition, NEXDINE has created a robust memory care dining program that goes above and beyond the traditional “food” component and creates an experience for our residents. This includes dining room ambiance, place settings, china, and how to differentiate our service techniques to accommodate this specific population.
Aromatherapy
Aromatherapy or the use of scents to promote healing, relaxation, and a sense of well-being is considered to be a complementary therapy to help enhance our residents’ dining experiences. According to several studies, smells can trigger positive emotional and autobiographic memories. Therefore, olfactory stimulation might be useful to improve the quality of life and well-being of people with dementia, so NEXDINE always strives to cook menu items in the memory care neighborhoods to create enticing aromas for the residents. Elderly patients or residents may experience a reduction in their sense of smell due to medications, illness, infection, or dementia. This results in a reduction of taste and flavor when consuming food and drink. However, a sense of smell is key for appetite stimulation and plays a role in triggering memories and influencing moods. Research indicates that there may be numerous benefits to aromas in the dining room. In addition to stimulating appetite and triggering memories, aromas can help provide relief from anxiety and depression and improve quality of life, particularly for people who have chronic health conditions, and may also relieve muscle pain, insomnia, and nausea. In fact, one study assessed the effect of olfactory stimulation on food intake, in which participants were exposed to a meat scent in the dining room for 15 min before serving the main course during two lunches that were alternated with the control condition (two scent-free lunches). A significant effect of the olfactory priming was found with a 25% increase in meat consumption and an increase in vegetable consumption approaching significance compared to the control condition. Behavioral observations also showed a significant increase in residents’ interest in the meal in the scent-primed lunch condition. Therefore, NEXDINE incorporates menu items that can trigger an olfactory response through freshly brewed coffee, homemade cookies and even making bread in the neighborhoods.
Music
Music can communicate, motivate, calm, or enliven, alleviate pain and anxiety, and lift spirits. It can also be used to provide sensory stimulation at mealtimes, enhancing the enjoyment of the meal and fostering improved intake and nutritional status. Research has shown that playing music in the dining room can help decrease stress levels and agitation, facilitate a pleasant and harmonious environment, and provide a cueing mechanism for the intake of foods and fluids. NEXDINE recommends selecting music that is relaxing and doesn’t contain lyrics, as sometimes residents will start to sing or dance to the music, creating a distraction for themselves and others. Some suggestions include piano music, calm classical music, upbeat dinner music such as Spanish guitar, and big band compilations. Staff can also speak with residents or patients and their family members to ascertain what music each resident finds most enjoyable.
Conversation Starters
Silence in the dining area detracts from an otherwise positive atmosphere. However, for residents with dementia, it can be difficult to hold a conversation. This is because recent memories are the first to deteriorate. While a resident may not be able to make small talk, they may be able to converse about their childhood, favorite pastimes, and other topics. Having conversation starters planned can help facilitate positive conversation. Therefore, NEXDINE has training surrounding conversation starters for staff to engage meaningfully with residents while they are dining within the dining rooms.
NEXDINE’s TASTEFUL Programming

TASTEFUL Textures is NEXDINE’s advanced texture-modified food program. Dysphagia and difficulty in swallowing are not uncommon in senior living or healthcare environments. Yet, many food and dining programs give little consideration to individuals with these conditions, heating and serving frozen, processed purees that address safety, but ignoring the dignity and enjoyment of the patient or resident. TASTEFUL Textures is a state-of-the-art program, based on the latest medical science and firmly rooted in our Culinary Values and commitment to fresh, authentic food made from scratch. Our program integrates the full spectrum of diet levels specified in the International Dysphagia Diet Standardization Initiative (IDDSI), and our teams are equipped with the tools, recipes, ingredients, and guidance to create texture-modified meals and exquisite purees that are artfully presented and served for residents or patients to enjoy with the confidence and dignity each deserves.

TASTEFUL Bites is NEXDINE’s approach to supporting individuals diagnosed with memory impairment such as dementia and Alzheimer’s. These individuals, like all NEXDINE customers, are deserving of an enjoyable dining experience that supports the adequate intake of quality nutritional meals and socialization. Memory care programs present a unique opportunity to enhance and develop new strategies specific to residents’ and patients’ needs. The foundational aspects of TASTEFUL Bites consider the needs of those with progressive memory decline related to food, nutrition, dining, and dignity. The program is designed to support independence during mealtimes and solutions to dexterity challenges.

TASTEFUL Plus: NEXDINE’s enriched foods and supplemental nutrition program for individuals who require added calories or protein. As the dementia resident requires increased nutrition our TASTEFUL Plus program allows residents or patients to enjoy scratch-made foods that meet their nutritional goals versus relying on commercial supplements like Ensure or Boost.

TASTEFUL Sips: NEXDINE’s enhanced hydration program. All people benefit from staying well hydrated, and TASTEFUL Sips makes hydration an experience especially as the elderly population has such a decline in fluid intake. We take hydration a step further to include house-made infused waters, teas, smoothies, fresh pressed juices, and even popsicles for an all-encompassing program.
NEXDINE has created a robust memory care dining program that goes above and beyond the traditional “food” component and creates an experience for our residents. Throughout each segment of our business, we have culinarians and Registered Dietitian Nutritionists that create individualized dining and nutrition programs for each client we serve. To learn more about NEXDINE Hospitality and the refreshing approach to dining management that is reshaping the industry with collaborative, innovative, customized dining programs and the most responsive and passionate team of dining and hospitality professionals, contact NEXDINE today.
Written by: Rebecca McCullough
SVP NHW NEXDINE Hospitality
References:
https://www.nia.nih.gov/health/what-do-we-know-about-diet-and-prevention-alzheimers-disease
https://alzres.biomedcentral.com/articles/10.1186/s13195-022-00957-1
https://www.medicalnewstoday.com/articles/mind-diet#purpose
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9243450/
